Emerging Healthcare Technology: Opportunities and Challenges for Healthcare Providers
Several notable technologies are driving the future of healthcare. As these technologies become more advanced and more commonplace, look for healthcare providers, organizations, and methods of care to evolve alongside them.
Emerging healthcare tech trends:
- Artificial intelligence (AI)
- Extended reality
- Digital therapeutics (DTx)
- Data analytics platforms
- Remote patient monitoring
- In silico methods
- Telehealth and virtual visits
Issues facing healthcare tech:
- Bias
- Data privacy
- Technology equity
- Lack of integration among systems
- Outdated legacy system
Artificial intelligence (AI)
AI in healthcare uses machine learning, data analysis, and sophisticated models to improve efficiency and health outcomes. AI is being used in healthcare in many ways—both for patient care and healthcare operations:
Patient care
- Medical image analysis
- Disease diagnosis and prediction
- Drug discovery and development
- Personalized treatment planning
- Electronic health record management
- Robot-assisted surgery
- Virtual nursing assistants
- Health monitoring through wearable devices
- Precision medicine
- Clinical decision support systems
Healthcare operations
- Patient scheduling and appointment management
- Inventory management
- Supply chain optimization
- Staff scheduling
- Workforce management
- Insurance fraud detection
- Billing and claims processing
- Predictive maintenance of medical equipment
- Revenue cycle management
- Patient flow optimization
- Resource allocation and capacity planning
- Data analytics for finances and operations
Researchers are exploring more potential uses for AI in medical physics, dermatology, cancer diagnostics, nuclear medicine, medical imaging, cardiovascular imaging, neuroradiology, psychiatry, dentistry, and other areas. However, there are still a few barriers to widespread adoption to overcome.
One barrier is consistent accuracy. AI-generated content has resulted in errors and “coherent nonsense”—something that is especially concerning in an area as complex and specialized as medicine. Healthcare organizations must continue to review and verify any information generated by AI tools. And luckily, the AI models and tools that use them are getting better by the day. For example, Med-PaLM is a large language model (LLM) from Google designed to answer complex medical questions. It is trained and tested using medical research, licensing exams, and real-world patient questions and interactions. When tested, the answers from Med-PaLM aligned with medical and scientific consensus 92.6% of the time.
Another barrier is the shifting regulatory landscape. Any new technology comes with challenges for regulators and professional organizations—and AI is certainly no exception. AI is evolving rapidly, and regulators want to ensure it is developed and used safely. The Artificial Intelligence Act from the EU, adopted in 2024, is one of the first major regulatory frameworks for AI—but it’s far from the last. The EU uses a phased, risk-based approach that implements restrictions on the highest-risk AI applications sooner than lower-risk applications.
Look for AI regulators to continue to balance fostering innovation with protecting the public: ensuring data privacy, validating AI algorithm accuracy, addressing bias, establishing liability frameworks, and adapting existing medical device regulations.
Extended reality
Extended reality (XR) is an umbrella term encompassing virtual reality (VR), augmented reality (AR), and mixed reality (MR) technologies. These immersive technologies are revolutionizing healthcare by offering innovative solutions for both patients and healthcare providers.
AR enhances the real world by overlaying digital imagery onto the user’s physical environment, typically viewed through smartphones, head-mounted displays, or heads-up displays (HUDs).
Mixed or merged reality takes AR a step further, allowing digital elements to interact with real surroundings, often controlled by users.
VR creates a fully immersive experience that replaces the user’s surroundings with a simulated, interactive virtual environment, usually accessed through a headset.
The applications of XR in healthcare are diverse and rapidly expanding. Mental health care, pain management, surgical assistance, diagnostics, patient communication, home healthcare, telehealth, and staff training are just a few areas benefiting from these technologies. The U.S. Food and Drug Administration (FDA) has already approved more than two dozen medical devices incorporating AR and VR technology.
One of the key advantages of AR and VR treatments is their portability and accessibility, making them suitable for diverse patient populations. This flexibility allows for wider implementation across various healthcare settings and demographics.
Specific examples of XR applications in healthcare include:
- Surgical assistance: AR technology can overlay medical images onto a patient during an operation, guiding the surgeon’s technique with enhanced precision.
- Mental health treatment: VR is used to treat post-traumatic stress disorder in military veterans by creating controlled, immersive environments for exposure therapy.
- Rehabilitation: VR simulations of real-life situations help improve physical functions for stroke survivors, enhancing their recovery process.
- Medical education: VR environments allow medical residents to practice patient interactions, improving their comfort level and skills before real-world application.
- Patient preparation: VR simulations of healthcare procedures or interactions can reduce anxiety in patients by familiarizing them with upcoming experiences.
As the field continues to evolve, expect to see even more innovative uses of AR, VR, and MR that further transform patient care, medical training, and healthcare delivery.
Digital therapeutics (DTx)
Digital therapeutics (DTx) is the use of high-quality software programs to prevent, manage, or treat a medical condition. It is scalable and cost-effective for providers to offer, and it is a more convenient way for patients to engage with their treatment plan.
Clinicians are using DTx to treat a wide range of conditions, including cancer, ADHD, migraines, insomnia, depression, and anxiety. Some DTx products deliver specific types of therapy, some use VR/AR, and others help patients track symptoms. DTx may be used independently or combined with other treatment methods.
These tools build on the success—and consumer expectations—of popular mobile health apps. Growing numbers of people use smartphone apps to track fluid intake, nutrition goals, medication use, and the symptoms of diabetes, hypertension, multiple sclerosis (MS), and other conditions. Along the same lines, more providers equip their home health staff with mobile apps devices with EHR support and patient care tools.
DTx technologies and apps will make healthcare more accessible to a wider range of patients, as long as medical providers, systems, and insurers are equipped to use them. This will be especially important in areas that are underserved by traditional health care services and in distributed care sites like mobile health clinics that have very limited space and equipment.
Data analytics platforms
Data analytics have never been more important in healthcare. Leading health organizations are looking for new and better ways to use their data to streamline operations and improve patient care.
This data comes from many sources, including databases, devices and sensors, transactions, medical records, and other documents. For example:
- Medical device makers analyze commercial data like buying behavior and inventory trends to manage inventory, field personnel, and shipping logistics.
- Medical providers track regulatory data like billing and coding accuracy, adherence to service level agreements (SLAs), and data security metrics.
- Healthcare organizations analyze operational data like service quality KPIs (e.g. patient satisfaction), employment KPIs (e.g. employee engagement), and efficiency data (e.g. workforce utilization and travel time).
Healthcare leaders are putting more emphasis on—and investment in—data analytics to stay competitive. Creating dashboards and automating reports for managers helps identify outliers and negative trends: underutilization of skilled workers, long wait times for certain types of service, high rate of uncollected patient payments, and key pieces of medical equipment nearing their average lifespan. Advanced analytics platforms are taking this to the next level, helping leaders uncover complex relationships between variables and data from different sources.
Remote patient monitoring
Remote patient monitoring (RPM) is a healthcare technology that enables the collection of patients’ health data outside traditional clinical settings. RPM tracks vital signs and key health markers, giving providers continuous insight into patients’ well-being and alerting them to concerning data points that need timely intervention.
Many consumers already use wearable devices or health trackers to monitor daily activities, sleep patterns, heart rate, blood sugar levels, and oxygen saturation. These tools offer real-time data that can help individuals manage their health more effectively. However, RPM takes this a step further by enabling healthcare providers to monitor patients’ vital signs. This is especially important after surgeries, cardiac events, or the start of a new treatment regimen. By tracking important health metrics, providers can catch potential complications early and adjust treatment plans as needed.
One of the major benefits of RPM is its integration with EHR, EMR, and PM systems. In highly integrated systems, vital signs and other health data collected from RPM devices are automatically recorded into digital patient records. This streamlines the documentation process, reduces the time clinicians spend on charting, and ensures data is up-to-date and accurate for better-informed clinical decisions.
As RPM continues to advance, it is expected to play an increasingly vital role in preventive care and chronic disease management. The future of healthcare will also likely see RPM integrate further with AI and predictive analytics for even more personalized care plans. With these developments, RPM will continue to increase patient access to high-quality healthcare.
In silico methods
In silico refers to computer-based methods to simulate, model, and analyze biological processes, diseases, and medical treatments. This approach uses algorithms, data analysis, and machine learning to perform experiments and conduct studies in a virtual environment. In silico methods may depend on simulations of living systems—for example, the HumMod model of human physiology uses more than 9,000 variables to simulate human systems.
In silico methods are increasingly used for:
- Drug discovery and development: Predicting drug efficacy and potential side effects before clinical trials.
- Disease modeling: Simulating disease progression and treatment outcomes.
- Personalized medicine: Tailoring treatments based on an individual’s genetic profile.
- Clinical trial optimization: Designing more efficient and targeted trials.
- Medical education: Creating realistic simulations for training healthcare professionals.
Ideally, in silico approaches will combine with in vitro and in vivo studies to open up new avenues of medical research. These methods will also complement the trend toward digital twins, precision care, and highly personalized treatment plans.
Telehealth and virtual visits
Telehealth and telemedicine have transformed the way healthcare is delivered by providing virtual options that extend beyond traditional in-person visits. Telehealth services include virtual visits, phone calls, remote consultations, and communication tools for patients to share updates and images.
Virtual care bridges the gap by offering a practical solution for routine check-ups, follow-ups, and even urgent care without the need for physical travel. This is a game-changer for communities with limited healthcare infrastructure and patients who can’t travel to centralized healthcare facilities.
Telemedicine can also complement in-person care. Providers can share virtual resources, such as educational videos, before a visit to help patients arrive more informed. This allows patients to better understand their condition and spend more appointment time discussing specific concerns and asking questions. The result is more productive in-person visits and more personalized care.
The growth of telehealth was accelerated by the COVID-19 pandemic, and it will continue to serve as an important and cost-effective part of patient care. Look for healthcare providers and software developers to pursue new technology-driven ways to expand patient access and engagement.
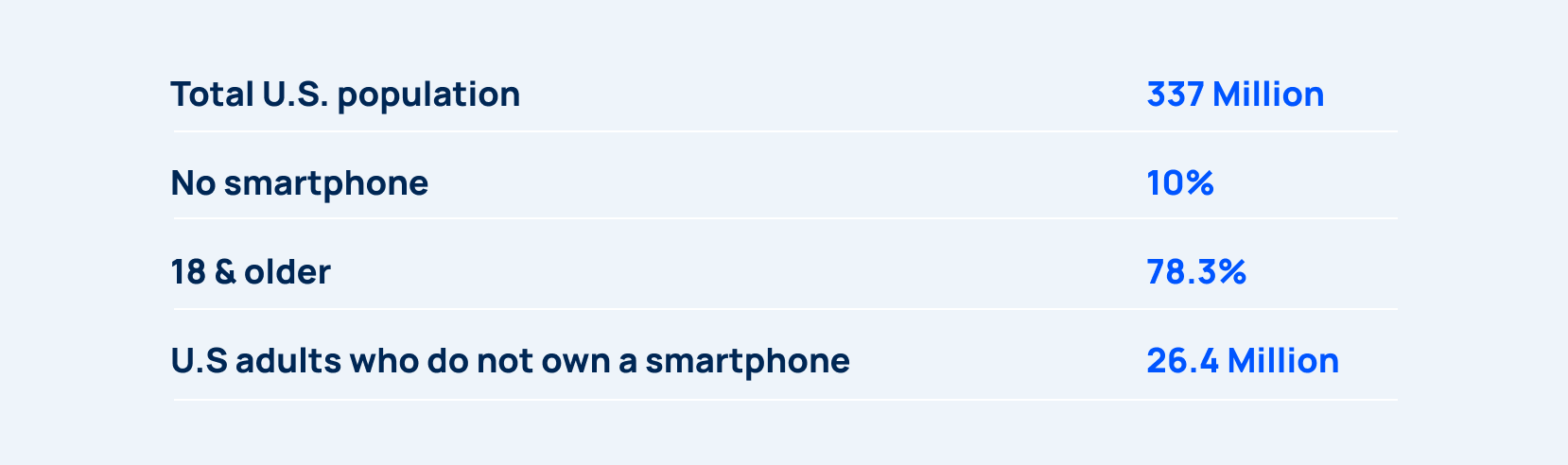
For example, it’s easy to say health tracking smartphone apps are available to “everyone.” After all, 90% of people in the U.S. have a smartphone! But that still leaves 26+ million adults in the U.S. without a smartphone. (If you consider people with limited data plans or older-model phones without Bluetooth capabilities, even more people are left out of healthcare tech solutions.)
A smartphone, network data plan, and reliable access to the internet makes a huge difference for health outcomes. For example:
- On a personal level, people miss out on health tracking apps, digital therapeutics, patient portals, insurance apps, online billing, and other tools that make it easier to get care.
- On a community level, people have a harder time securing jobs and accessing community resources (e.g. a local nonprofit announces pickup locations on social media for food, baby care, clothing, etc.) that affect their overall health and well-being.
- On an organizational level, providers have a harder time engaging patients using digital portals, telehealth tools, and online communications.
- On a government level, public health agencies must work harder to spread news and guidance about public health emergencies and safety hazards, and people most at risk of certain illnesses are least likely to be included in digital contact tracing.
Smartphones, health tracking apps, patient portals, and public health tracking have changed healthcare—but only for those who can participate. This is important to keep in mind when designing healthcare workflows that are increasingly technology-driven. Healthcare organizations and consumers without access to technology will improve patient outcomes much slower—if at all—compared to providers and patients with reliable tech. This can worsen the gap between the quality of healthcare available at different income levels and in different regions.
Lack of integration among systems
In an ideal world, the digital systems used by healthcare providers—EHRs, EMRs, and practice management software, among others—would communicate seamlessly. However, many of these systems remain siloed.
This lack of integration poses a significant challenge to healthcare providers. Without a unified view of patient data, providers risk ordering redundant tests, encountering conflicting information, and delaying timely treatment.
The burden often falls on patients to act as intermediaries, repeating their medical histories and navigating multiple patient portals to piece together their healthcare journey. This fragmentation hinders care coordination, increases administrative burden, and ultimately diminishes the patient experience.
Outdated legacy systems
Many organizations rely on legacy systems that are ill-equipped to handle the demands of modern healthcare. These outdated systems are often built to manage patient data, rather than support end-to-end healthcare operations. As a result, legacy systems struggle to accommodate the shift toward mobile workforces, remote patient monitoring, and real-time data analysis. Without updated technology infrastructure, an organization is less able to adapt to evolving patient needs, implement new technologies, and capitalize on a truly connected healthcare ecosystem.
Capitalize on emerging tech with the right investments
Emerging healthcare technologies present incredible opportunities and complex challenges for healthcare providers. As the industry evolves, healthcare organizations must embrace innovation, interoperability, and user-friendly technology to keep pace with rising patient expectations and a competitive market.
However, simply adopting new tools is not enough. Healthcare leaders must be mindful of existing technology disparities and concerns about bias, privacy, and security of emerging technology like AI.
Skedulo is helping healthcare organizations embrace the future of tech-enabled care through automated scheduling, smart optimization, and workforce management tools. The Skedulo Plus app allows healthcare providers to create custom workflows that meet the needs of their practice. Skedulo integrates with Epic EMR systems, Workday, Zendesk, and many other tools—from HR systems to billing to payroll—to extend the capabilities of existing systems.
To learn more about the future of healthcare, check out AI Trends: What to Expect in the Years Ahead and Trends In The Shifting Point of Care.